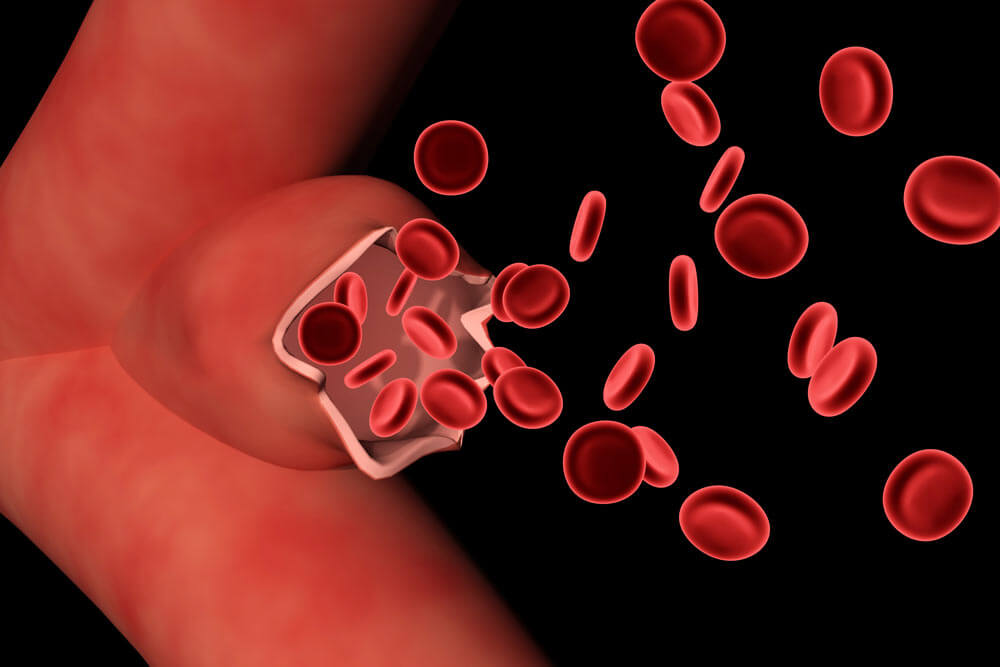
When the wall of a blood vessel weakens, a balloon-like dilation called an aneurysm sometimes develops. This happens most often in the abdominal aorta, an essential blood vessel that supplies blood to your legs.
Fairly common
Every year, 200,000 people in the U.S. are diagnosed with an abdominal aortic aneurysm (AAA).
A ruptured AAA is the 15th leading cause of death in the country, and the 10th leading cause of death in men older than 55.
Family history is important
Aneurysms run in families. If a first-degree relative has had an AAA, you are 12 times more likely to develop an abdominal aortic aneurysm. Of patients in treatment to repair an AAA, 15–25% have a first-degree relative with the same type of aneurysm.
Symptoms
May be absent
In most cases, abdominal aortic aneurysms cause no symptoms and are found when you are being evaluated for another medical condition.
Sudden, severe abdominal or back pain
If you have a family history of AAA and feel sudden, severe pain in your abdomen or back, seek immediate care. These symptoms may signal that you have developed an AAA, possibly one in process of rupturing.
Pain, discolored skin, sores on feet and toes
A small percentage of patients with AAA have these symptoms when plaque or blood clots from elsewhere in the body collect in the feet and toes.
Causes
Many factors contribute to AAA formation.
- Some type of inflammation that causes a weakening of the wall of the aortic artery.
- Men older than 60, smokers, Caucasians and anyone with a first-generation relative who has developed an AAA are at highest risk for an abdominal aortic aneurysm.
- Age (50+ for men, 60+ for women) and a history of atherosclerosis, high blood pressure, elevated cholesterol, heart or peripheral vascular disease and tobacco use are all associated with AAA formation.
- Other potential factors associated with AAA formation include tears in the arterial wall, infections, and congenital connective tissue disorders.
Diagnosis
You may need to see a vascular surgeon.
Most AAAs cause no symptoms and are found incidentally, during an evaluation for another medical condition. If you are affected, see a vascular surgeon.
Imaging tests may be needed
An abdominal ultrasound is painless, cost-effective, safe and the most frequently utilized test to screen for and measure the size of an AAA.
Computed tomographic angiography (CTA) will assess aneurysm size, location and the extent of impact. This study requires exposure to radiation and injection of an intravenous contrast agent. However, a CTA provides valuable anatomic information and can help your vascular surgeon determine the optimal type of repair.
Treatments
Treatment depends on the size of the aneurysm.
Small AAAs (less than 5 cm in diameter)
have a very low risk of rupturing, but should be watched.
- It’s important to have an ultrasound test every 6–12 months to monitor for aneurysm growth and risk of rupture.
- Lifestyle changes that help control blood pressure and medication may help you.
- If you smoke, ask your vascular surgeon to help you find a smoking cessation program that will work for you.
- Daily exercise is also beneficial.
Larger (more than 5.0-5.5 cm in diameter)
rapidly enlarging and AAAs causing symptoms are usually repaired.
Open surgery requires placement of a prosthetic graft.
- The vascular surgeon accesses the affected portion of the aortic artery through an incision in your abdomen.
- Most patients stay in the hospital 4–10 days. Recovery time may be up to 3 months.
Endovascular aneurysm repair (EVAR) is a less invasive treatment.
- Two small groin incisions are made. Guided by X-ray imaging, the vascular surgeon introduces a tiny device into the artery. The device is used to reinforce the artery wall and exclude the aneurysm.
- Most patients stay in the hospital 1–3 days. Recovery time is shorter than with open surgery.
Staying Healthy
- Know and share your family history. If you are diagnosed with an abdominal aortic aneurysm, educate first-generation relatives of their increased risk.
- If you smoke, ask your vascular surgeon to help you find a smoking cessation program that will work for you.
- Follow a healthy, low-sodium diet.
- Maintain a healthy weight.
- Get regular exercise.
- Have your blood pressure and cholesterol checked regularly.
- Ask your primary care physician to evaluate you for medications to control your blood pressure, lower cholesterol levels and/or thin your blood.